Thickening of the heart muscle: genetic testing can help the entire family
There are a number of possible causes for thickening of the heart muscle. High blood pressure is the most common cause of a thickened cardiac muscle. If the thickening of the muscle is genetic, it may cause major problems in individual patients. Genetic testing can provide important additional information when it comes to early treatment – for yourself and for your closest family members, says cardiologist Dr Peter Burger.

Heart disease is often linked to increasing age or an unhealthy lifestyle. But you also encounter young patients over and over ...
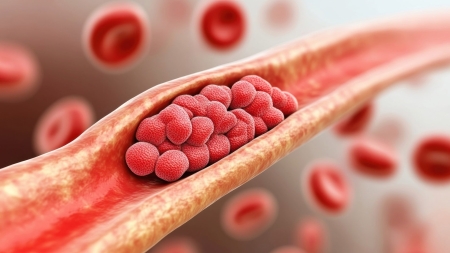
That’s right. The most common heart problem by far is coronary heart disease, i.e. a disease of the cardiac vessels. Due to existing risk factors such as high blood pressure, obesity, diabetes, elevated blood lipids or smoking, these can become narrower with increasing age and lead to a heart attack.
However, thickening of the heart muscle is a problem that can become noticeable as early as puberty, although the symptoms experienced by the patients affected vary greatly. The progression of the disease known as cardiac muscle hypertrophy (hypertrophic cardiomyopathy - HCM or hypertrophic obstructive cardiomyopathy - HOCM) is also highly individualised. In the majority of patients, the disease is benign. However, things can also proceed very differently.
Could you describe it in more detail?
With pleasure. It was an unusual case because the 49-year-old patient was originally hospitalised for lumbago and the thickening of the heart muscle was discovered by chance during the examination. While performing a more detailed routine physical examination, we found that the man had a heart murmur and an abnormal resting ECG. An ultrasound examination of the heart revealed a severe thickening of the heart muscle, which among other things led to a malfunction of the heart valves and obstructed the flow of blood from the heart. The diagnosis of a thickening of the heart muscle (HOCM) was subsequently confirmed by magnetic resonance imaging (MRI).
The patient had apparently been living with this condition for some time. How did the patient get on after this diagnosis?
Quite well, actually. His condition remained relatively stable for the next five years. After that, however, the patient began to complain increasingly of shortness of breath when exerting himself and eventually also of chest pain, which did not improve despite taking medication. An ultrasound revealed that the heart muscle had thickened further. Blood could no longer flow between the left ventricle and the aorta properly. In addition, there was an increased backflow between the left ventricle and the left atrium via the heart valve. We ended up having to perform surgery to remove several layers of the heart muscle and insert a heart valve. The patient has been doing well since then, however. His shortness of breath and chest pains have gone away.
Why did you nevertheless advise the patient and his siblings to undergo genetic testing? After all, his three brothers and two sisters had no known heart problems.
It is unusual for a young patient to suffer from thickening of the heart muscle. It always makes me sit up and take notice. I immediately suspect that the cause may be genetic. If you know which gene is responsible for the disease, you can search for this gene among the patient's closest relatives (siblings, children, and possibly also parents, uncles and aunts) using relatively simple blood tests. If the corresponding gene is identified, close monitoring and, where necessary, treatment are recommended. Even if patients often do not realise they have been living with the disease for a long time, they would nevertheless benefit from early treatment.
What did the genetic testing show?
The obligatory consultation prior to genetic testing already indicated that the patient had a genetic predisposition: his father died at 74 – presumably from heart failure. One of the patient's sons also had a severe thickening of the heart muscle at the age of 19. The other son was diagnosed with a slight thickening of the heart muscle at the age of 24. After obtaining confirmation that the costs would be covered, my patient underwent genetic testing. The researchers analysed 78 genes related to the cardiac muscle. We identified a variation in the MYH7 gene, which was subsequently also found in one of his sons.
What is the significance of this genetic variation?
Changes (mutations) in the MYH7 gene and changes in the MYBPC3 gene are responsible for around 40 per cent of hereditary thickening of the cardiac muscle. Several hundred variations that can lead to these changes have already been identified.
What does genetic testing mean for treatment?
Because the progression of hereditary enlargement of the cardiac muscle is highly individual, the result in itself does not allow for improved treatment. In my opinion, the greatest advantage is that all family members with an increased risk of an enlarged heart muscle can request a genetic test (cascade screening): people who are not carriers of a conspicuous genetic variation can therefore be exempt from regular heart check-ups, while carriers of variations would need to have their heart examined regularly via ultrasound and ECG in order to be able to react quickly to any changes. In particular, people with a genetic thickening of the cardiac muscle should refrain from participating in competitive sports. In addition, there may soon be a drug available in the form of Mavacamten that can also have a positive effect on the progression of the disease.